A Wireless Plant to Fight Glioblastoma
Normally we do not publish news related to the pre-clinical phase but this seems very interesting for the potential impact on treatments, especially if in combination with the other treatments in use.
Imagine that a patient’s brain tumor can be treated painlessly, without anesthesia, in the comfort of his home. For now, Stanford Medicine researchers have developed and tested a small wireless device in mice that is activated remotely and is able to heat the nanoparticles injected into the tumor site, gradually killing only the cancerous cells.
In mice with brain tumors, 15 minutes of treatment per day over 15 days, while the animals were doing their normal activities, was enough to significantly increase survival times. The researchers just published their work in Nature Nanotechnology.
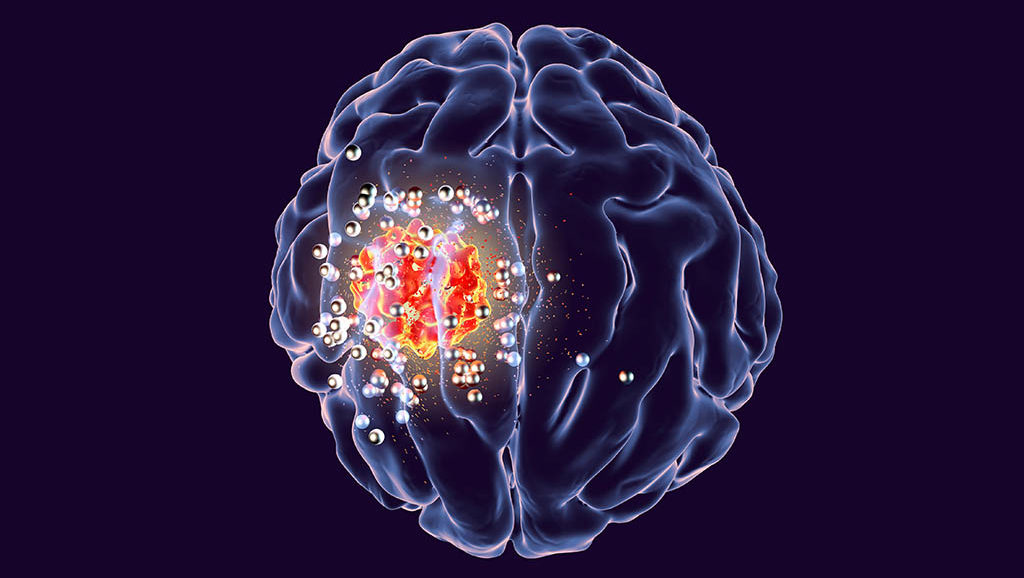
The nanoparticles help target treatment only at the tumor site and therefore side effects will be less than with chemotherapy and radiotherapy. The treatment uses a principle similar to that of hyperthermia often used as an adjunct treatment by some patients with glioblastoma.
In this case it is a photo-thermal treatment that uses light to heat the nanoparticles. The team of researchers have developed a small wirelessly powered device that needs to be implanted between the skin and the skull. Specially designed gold nanoparticles are injected into the tumor through a tiny hole in the skull. When turned on, the device emits infrared light that can penetrate brain tissue to activate the nanoparticles, which consequently raise the temperature by up to 5 degrees Celsius. This is enough to kill cancer cells with repeated treatments without damaging the surrounding brain tissue.
By regulating the power and wavelength of light, researchers can target tumors of different sizes and locations in the brain. The structure and dosage of the nanoparticles are calibrated to generate the right amount of heat.
The researchers tested their device on mice that had brain tumors of human origin implanted. Mice were not affected by the device as short and limited warming in a clinically acceptable range does not affect normal activities. The researchers also verified that the injected nanoparticles remained at the tumor site and did not endanger the surrounding tissues.
Treated mice lived significantly longer than untreated mice, with average survival times doubled and sometimes tripled. When the new treatment was combined with chemotherapy, the mice lived even longer.
The researchers predict that their device, when adapted to human patients, could be used for home treatment in addition to surgery, chemotherapy or radiation, without increasing the burden of hospital visits. Researchers are confident they will adapt the device to humans in less than five years.